1.2 Your business case
Once you’ve embraced the patient-centered promise of sDHTs, the next step is building a compelling business case that unlocks efficiencies, returns, and competitive advantages in medical product development.
It’s one thing to see the scientific promise of sDHT adoption; it’s another to turn that vision into a rock-solid business rationale that will convince your team, leadership, and stakeholders that this is worth the investment.
The good news is that a growing body of analyses, real-world examples, and economic modeling indicate that adopting sDHTs can offer meaningful operational and financial advantages when applied in the right context. While outcomes vary by program and assumptions matter, these approaches increasingly support credible, data-driven business cases for investment in digital endpoints.

OVERVIEW
Digital endpoints drive value
In most companies, the push for digital endpoints starts with a clinical need, like capturing more nuanced data on patient outcomes to show benefit or identify new opportunities for therapeutic intervention.
To scale it across trials, speak the language of value—dollars, timelines, and competitive edges. Organizations that advance this shift capture significant advantages, unlocking value for shareholders and patients alike.
Consider the acceleration factor
sDHT precision means trials detect treatment effects faster and with greater confidence, shortening durations by months. For adopters, this translates to earlier market entry, first-mover advantage, and millions in increased Expected Net Present Value (eNPV).
From cost to value: The ROI of sDHTs
The upfront costs associated with integrating technology, training teams, and validating endpoints can be offset under the right conditions. In late-stage trials, adopters may realize 4-to-6-fold ROI when sDHTs enable reductions in sample size, site visits, or operational complexity. Framing these investments in terms of potential value creation, rather than immediate cost, can support more productive discussions with finance and leadership teams.
sDHTs reduce participant burden and enable decentralized trials that reach broader populations, building trust with communities, regulators, and payers. Your products stand out by demonstrating meaningful improvements in real lives. This narrative resonates in boardrooms and beyond.
IN PRACTICE
The cost of standing still
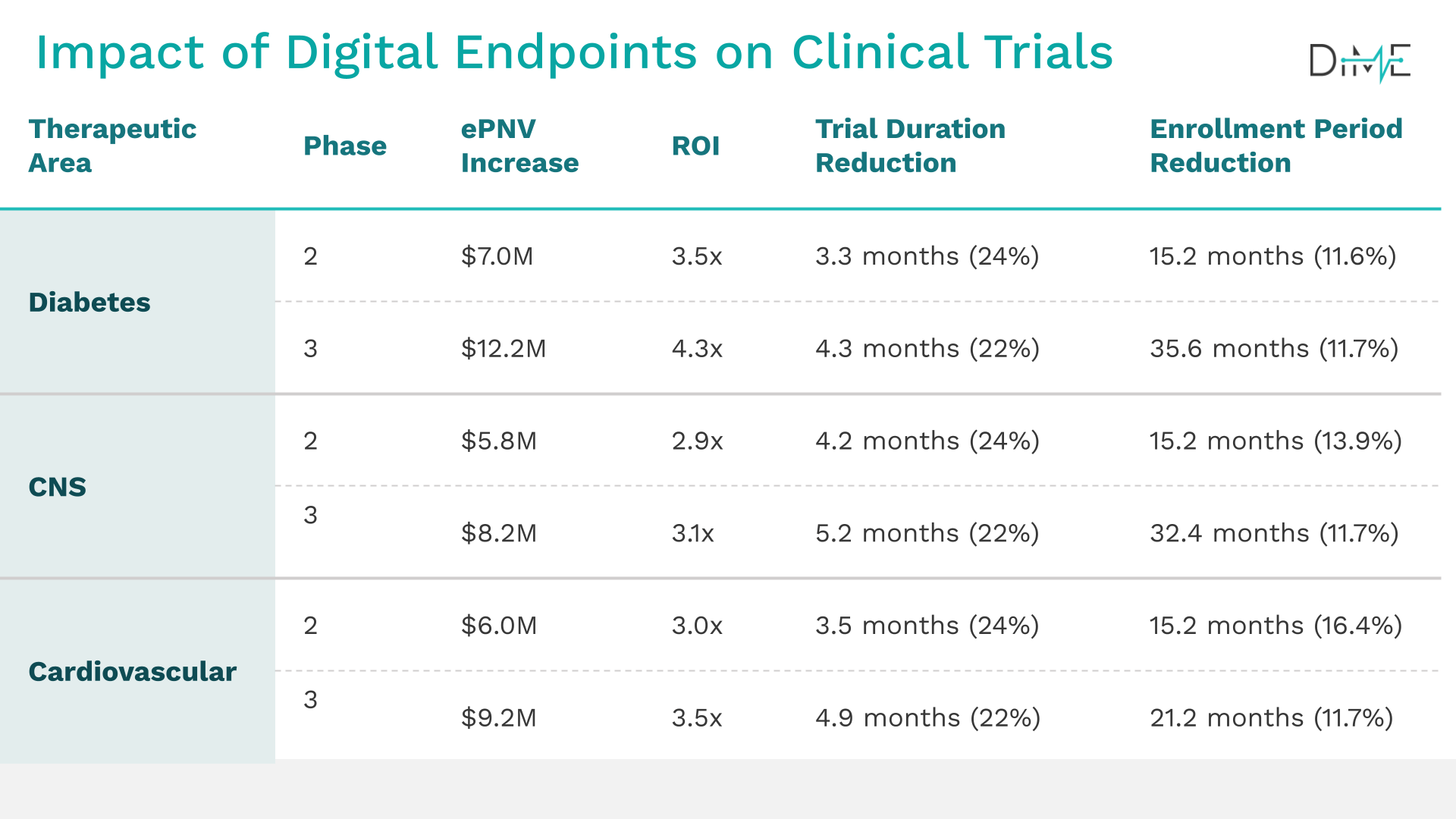
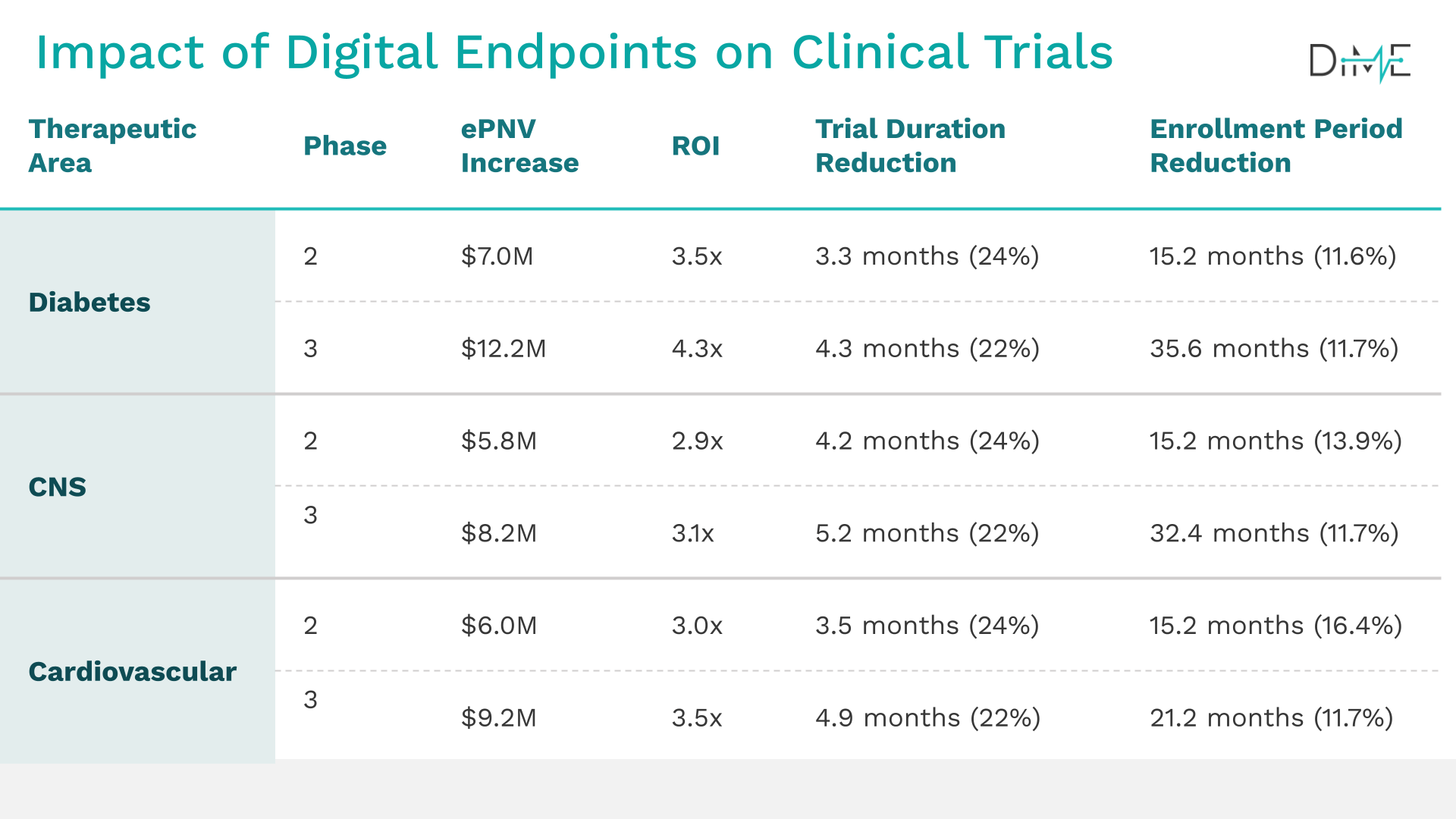
Financial impact by development stage
Calculate your eNPV with DiMe’s Digital Endpoints ROI calculator
Lead with value, frame with evidence. Building a digital endpoint is only half the battle—the other half is convincing your organization that it will pay off.
Use this interactive, evidence‑backed model (co‑developed with Tufts University CSDD and 10 leading sponsors) to quantify the economic upside of your specific trial design and therapeutic area. The ROI calculator turns industry benchmarks into a program‑level business case you can bring to finance, clinical, and C‑suite stakeholders in minutes.
PRO TIP
Benefits of digital in your trial
Competitive speed
Remote data capture and digital endpoints cut months from development timelines, accelerating first‑to‑market advantage.
Improved patient access
Decentralized designs reach participants previously excluded by geography, mobility or work constraints. Automated data collection can lower participant burden.
Higher quality signals
Longitudinal, frequent or continuous real‑world data improve sensitivity to change, reducing sample sizes or shortening trial duration.
Financial wins
Adopters that embed digital endpoints have already demonstrated 4‑ to 6‑fold ROI in Phase III and $27–40 M incremental eNPV per indication, driven by shorter cycle times and leaner sample sizes.
Action plan

Adopters: shaping internal and external buy-in
Next steps
Start by quantifying what’s at stake
Lean on tools like DiMe’s ROI Calculator and Value Framework to model out the efficiencies. By grounding your pitch in these data-driven projections alongside your program’s specifics, you make a persuasive argument that this isn’t speculative—it’s a smart allocation of resources.
Don’t stop at the numbers
Connect financial benefits to patient and scientific impact. Highlight how the endpoint expands trial access, lightens the load on participants, boosts inclusivity and access, and yields richer, ongoing data that paints a truer picture of real-world outcomes. These elements resonate with clinicians, patient advocates, and regulators, showing that the upside goes far beyond the balance sheet to create lasting value in how we develop therapeutics and products.
Pull it all together
Foster alignment early (see Section 2.3: Stakeholder alignment). Bring in voices from clinical, statistical, data science, regulatory, patient engagement, operations, and finance for a dedicated stakeholder workshop. This collaborative step uncovers shared priorities and heads off any silos that could cause friction later. Involve regulatory experts early to identify evidence needs and opportunities, saving significant time and preventing rework. (See Section 3: Engage Regulators).

Developers: your contributions to building the business case
While adopters typically lead on the financial and operational framing for integrating an sDHT into a trial, you as a developer bring essential insights that bridge the conceptual vision with technical reality, ensuring the endpoint isn’t just aspirational but ready for the demands of real-world deployment.
Next steps
Collaborate with adopters in linking meaningful aspects of health (MAHs) to concepts of interest and potential endpoints (as covered in Section 2.1: Patient-informed endpoints).
Guide the conversation with feasibility details that shape expectations without overwhelming. Share key parameters that influence everything from processing costs to participant experience and site workflows. Be upfront about the resources needed to get trial-ready, whether that’s additional validation studies, data integration setups, or partnerships. Surfacing these early helps craft a budget and timeline that’s comprehensive and realistic.
When you and adopters merge your technical expertise with their organizational lens, the result is a business case that’s not only compelling but truly executable, setting the stage for smoother collaboration ahead.
When you and adopters merge your technical expertise with their organizational lens, the result is a business case that’s not only compelling but truly executable, setting the stage for smoother collaboration ahead.
AI is accelerating—not replacing—sensor‑based measurement
Artificial intelligence (AI) is transforming how sensor signals become clinically meaningful insights. AI cleans noisy data in real time, adapting algorithms, and revealing “digital phenotypes” that are difficult to see otherwise. This shift makes sDHTs more powerful than ever.
However, the foundational steps of sDHT adoption—such as patient-centered design, V3+ validation, and early regulatory engagement—remain essential. Adopters and developers will need to address AI-specific questions related to algorithm transparency or performance across subgroups, but AI does not lower the bar for validation or oversight; rather, AI becomes an important and powerful addition to the existing validation and evidentiary pathways to medical product development.
1.2 YOUR BUSINESS CASE
Library resources to guide you
The sDHT roadmap library gathers 200+ external resources to support the adoption of sensor-based digital health technologies. To help you apply the concepts in this section, we’ve curated specific spotlights that provide direct access to critical guidance and real-world examples, helping you move from strategy to implementation.
Gathers real-world examples, case studies, best practices, and lessons learned from peers and leaders in the field relevant to this section. Use these insights to accelerate your work and avoid common pitfalls.